Can Nattokinase or Lumbrokinase Help Break Down Microclots?
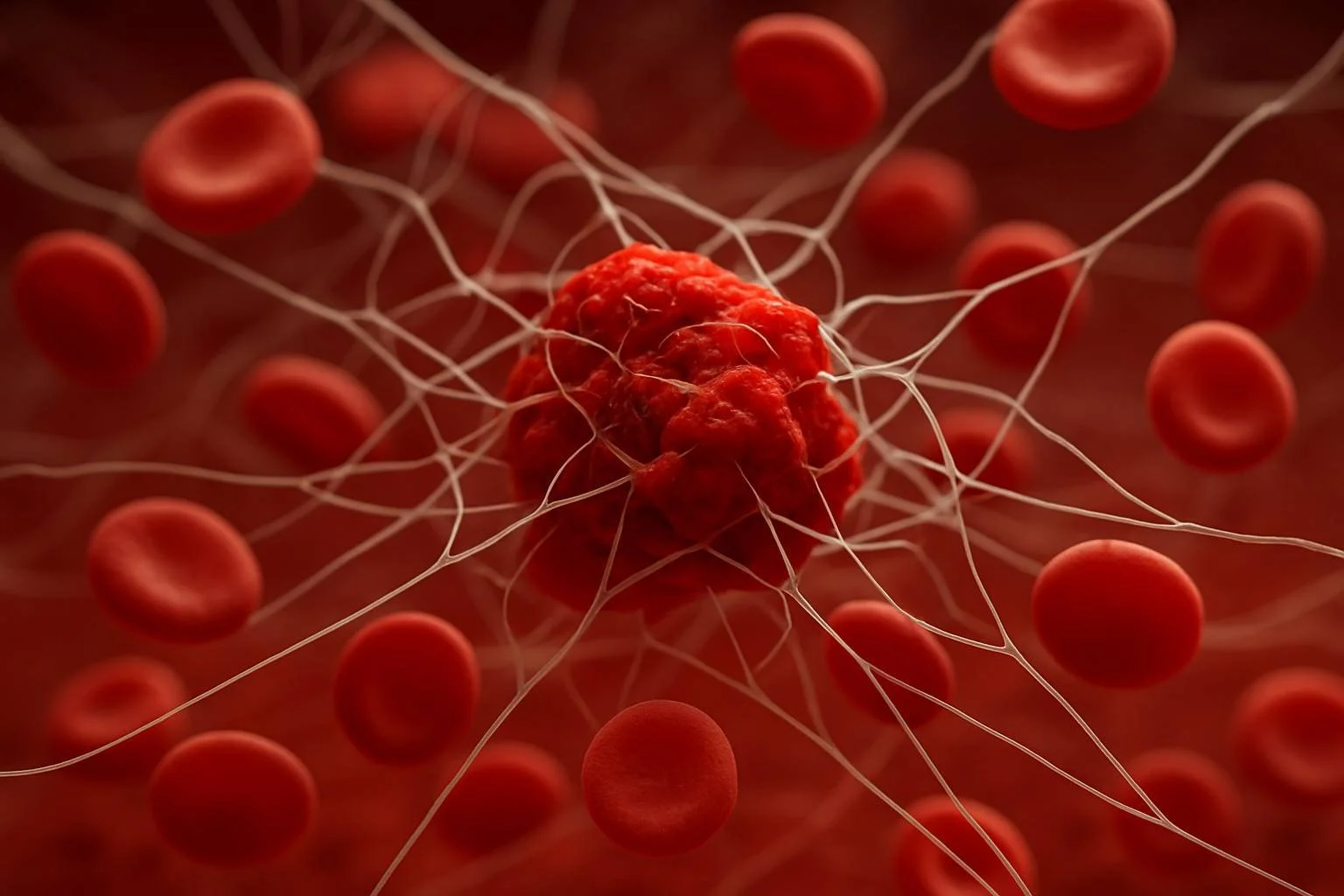
People with long-term COVID and ME/CFS have been found to have tiny clots called microclots. The fibrin used to form these clots is abnormal and difficult to break down. Microclots can decrease oxygen flow, obstruct tiny blood vessels, and potentially account for symptoms like post-exercise malaise (PEM), brain fog, and exhaustion.
Early research showed that people with long COVID and ME/CFS have microclots (Pretorius et al., 2021; Pretorius et al., 2023). This points to a possible shared problem with blood flow in both conditions.
Two naturally occurring enzymes—lumbrokinase from earthworms and nattokinase from fermented soybeans—have drawn interest as researchers search for methods to break up these microclots. These enzymes aid in the breakdown of fibrin. They are being researched as a potential means of enhancing blood flow in patients with chronic illnesses.
However, things like bioavailability, dosage, and mode of administration affect whether they truly work and how well the body absorbs them. This article will examine the scientific evidence regarding the use of lumbrokinase and nattokinase to treat microclots in patients with long-term COVID and ME/CFS.
What are Microclots?
Microclots are tiny, abnormal clots made mostly of a protein called fibrin. Unlike regular clots that the body can break down through a process called fibrinolysis, microclots are different. They are denser, harder to dissolve, and often trap inflammatory molecules like α2-antiplasmin and serum amyloid A. These substances block the body’s normal ability to clear clots (Pretorius et al., 2021).
Microclots don’t show up on standard blood tests or imaging. Detecting them requires special lab techniques, like fluorescence microscopy. Researchers have found these persistent clots in people with long COVID and, more recently, in those with ME/CFS (Pretorius et al., 2023).
Their presence is thought to block microcirculation—the flow of blood through the smallest vessels. This can reduce oxygen delivery to muscles and the brain, which may help explain common symptoms like exercise intolerance, fatigue, and brain fog.
These microclots are not harmless. They appear to trigger a cycle of oxidative stress, immune dysfunction, and blood vessel damage. Chronic inflammation and increased clotting tendency—both common in postviral conditions—may be what causes them to form in the first place (Laubscher et al., 2021).
While researchers are still working to understand whether microclots are a root cause or a consequence of illness, they remain a promising therapeutic target in long COVID and ME/CFS.
Why Microclots Matter in Chronic Illness
Microclots aren’t just a side effect—they may play a central role in ongoing symptoms in ME/CFS and long COVID. These small, hard-to-break-down clots can block the tiniest blood vessels, reducing the flow of oxygen and nutrients to cells (Pretorius et al., 2021). When tissues don’t get enough oxygen, it can lead to widespread problems, including fatigue, brain fog, and post-exertional malaise.
In ME/CFS, studies have shown poor oxygen use during exercise, low brain blood flow, and signs of metabolic stress. Microclots may help explain these findings by physically blocking the capillaries that supply oxygen to the brain and muscles (Wirth & Scheibenbogen, 2020).
In people with long COVID, researchers have found microclots in nearly every patient tested. These clots are linked to how severe the symptoms are, and they often remain in the blood long after the virus is gone (Grobbelaar et al., 2021).
One reason microclots are especially harmful is that they may trigger a vicious cycle. When blood flow drops, tissues become stressed and inflamed. This stress can further increase clotting, creating a self-sustaining loop of damage. Over time, this may explain the relapsing or worsening nature of symptoms in postviral illness.
While we still don’t fully understand why microclots form in some people and not others, we do know they can contribute to vascular blockage, immune activation, and oxidative stress. That makes them a logical target for treatment, especially for people who haven’t improved with other interventions.
Fibrinolytic Enzymes: A Natural Approach to Microclot Breakdown
Microclots are not easily broken down by the body’s natural enzymes. They’re also hard to treat with common blood thinners like warfarin or DOACs (direct oral anticoagulants), which mainly prevent new clots rather than breaking down existing ones.
That’s why some researchers are turning to fibrinolytic enzymes—natural compounds that help break down fibrin, the protein that forms the backbone of blood clots. These enzymes don’t thin the blood in a general way. Instead, they work by targeting and breaking down abnormal clots that resist the body’s usual clean-up process.
Two of the most studied enzymes for this purpose are:
Nattokinase, made from fermented soybeans
Lumbrokinase, extracted from earthworms (Lumbricus rubellus)
Both are taken orally and can be absorbed into the bloodstream, where they act as systemic fibrinolytics. Though they share some similarities, they differ in how specifically they act on fibrin, how long they stay active in the body, and how well they’re absorbed.
What the Research Shows
Nattokinase has been shown to break down fibrin, lower blood thickness (viscosity), and dissolve clots in animal and human studies (Sumi et al., 1987; Dabbagh et al., 2022). It may also reduce levels of proteins involved in clotting.
Lumbrokinase not only breaks down fibrin but also helps the body activate plasmin, a key enzyme in the clot-dissolving process. It seems to work more selectively than nattokinase, targeting fibrin without affecting other parts of the blood clotting system. This may lower the risk of bleeding (Zhang et al., 2013).
These enzymes are not standard blood thinners—they work differently. Their ability to dissolve resistant fibrin structures makes them especially interesting for treating microclots in chronic illness. While studies in long COVID and ME/CFS are limited, early lab research and clinical use suggest they may have real potential.
Still, for these enzymes to work, they must be absorbed into the bloodstream intact. Their effectiveness depends on the formulation, timing, and digestive health of the person taking them. Keep reading to learn more about that topic…
Nattokinase: What the Research Says
Nattokinase is a natural enzyme made by Bacillus subtilis during the fermentation of soybeans into natto, a traditional Japanese food. First discovered in 1987, it has since been studied for its ability to break down fibrin, the main protein involved in blood clots (Sumi et al., 1987). It’s now gaining attention as a potential treatment for microclots in long COVID and ME/CFS.
How It Works
Nattokinase helps dissolve clots in two ways:
It breaks down fibrin directly.
It boosts the body’s own clot-dissolving enzyme, called tPA (tissue plasminogen activator) (Hsu et al., 2009).
Studies also show that nattokinase can lower clotting-related proteins (Kim et al., 2008). This suggests it not only dissolves existing clots but may help reduce new clot formation as well.
Lab and animal studies support its use for dissolving both typical clots and fibrin aggregates that resemble the microclots seen in chronic illness. One small human study also showed improved blood markers related to clot breakdown after 8 weeks of nattokinase supplementation (Kurosawa et al., 2005). However, there are no published studies yet in long COVID or ME/CFS.
Can You Just Eat Natto Instead?
Not exactly. While natto does contain nattokinase, the amount varies widely and is usually much lower than what’s found in supplements. Also, the enzyme in food form is destroyed by stomach acid before it reaches the bloodstream.
For therapeutic use, standardized nattokinase supplements are more reliable. These products are usually enteric-coated to protect the enzyme and help with absorption.
That said, natto is still a healthy food! It contains vitamin K2, beneficial microbes, and polyamines, which may support overall cardiovascular health. But it’s not a substitute for clinical-grade nattokinase in managing chronic microclotting.
Nattokinase Evidence Summary
Increases fibrinolytic activity in humans after oral intake, even with a single dose (Sumi et al., 1987; Kurosawa et al., 2005)
Lowers clotting-related proteins like fibrinogen, factor VIII, and PAI-1 in human trials (Kim et al., 2008)
Promotes tPA release and breaks down fibrin directly in lab studies (Hsu et al., 2009)
No published trials yet in ME/CFS or long COVID, but the mechanisms align with microclot pathology
Lumbrokinase for Microclots: A More Targeted Enzyme Treatment
Lumbrokinase is a group of enzymes extracted from the earthworm Lumbricus rubellus. While the idea of using earthworm-derived enzymes might seem unusual, lumbrokinase has been studied for its ability to dissolve fibrin, the key protein involved in blood clots, for a very long time.
How Lumbrokinase Breaks Down Microclots
Lumbrokinase works through two main mechanisms:
Direct fibrinolysis – it breaks down fibrin directly.
Plasminogen activation – it helps the body produce plasmin, a natural clot-dissolving enzyme (Zhang et al., 2013).
Unlike pharmaceutical blood thinners, lumbrokinase appears to be more selective, targeting fibrin without interfering with other clotting factors. This reduces the risk of bleeding, which is especially important in chronic illness populations (Yan et al., 2015).
How to Take Lumbrokinase and Nattokinase for Microclots
Like nattokinase, lumbrokinase must be absorbed into the bloodstream to have systemic effects. That means formulation and timing are key.
Choose enteric-coated capsules – these protect the enzyme from being destroyed by stomach acid.
Take it on an empty stomach – ideally 45–60 minutes before eating or 2 hours after meals.
Some clinical reports suggest lumbrokinase may be more potent or longer-lasting than nattokinase. However, there are no direct comparison studies in humans yet.
Bioavailability of Fibrinolytic Enzymes in Long COVID and ME/CFS
For those using enzymes to treat microclots in long COVID or ME/CFS, bioavailability makes or breaks the outcome. If these enzymes aren’t absorbed properly, they won’t reach the bloodstream to break down microclots.
This is why formulation matters more than brand marketing. Look for:
Clinically studied products (e.g., Boluoke® for lumbrokinase, NSK-SD® for nattokinase)
Enteric-coated capsules with known activity in fibrinolytic units (FUs)
Guidance from a provider experienced in systemic enzyme therapy
From Earthworms to Evidence-Based Therapy
The use of earthworm-derived enzymes has deep roots in traditional Chinese medicine, where it has long been used to improve circulation. Today, modern lumbrokinase supplements are refined, purified, and tested under pharmaceutical standards. They’re far removed from traditional remedies—but still reflect the same principle: improving blood flow by breaking down hidden clots.
Best Way to Take Nattokinase and Lumbrokinase for Microclots
Just like with so many other supplement interventions, how and when you take fibrinolytic enzymes is critical. These are enzymes (a type of protein), and like all proteins, they can be broken down by stomach acid before they reach the bloodstream. For either to work throughout the bloodstream, they must be taken in the right form and at the right time.
Enteric Coating and Bioavailability of Fibrinolytic Enzymes
Enteric-coated capsules protect enzymes like nattokinase and lumbrokinase from stomach acid. Without this coating, the enzymes may be destroyed before they can enter circulation.
Studies in healthy adults show that fibrinolytic activity increases in the blood only when enteric-coated enzymes are taken on an empty stomach (Zhao et al., 2018; Kurosawa et al., 2005).
When to Take Enzymes for Best Results
To maximize bioavailability and effectiveness:
Take 45–60 minutes before eating, or
At least 2 hours after a meal
Food, especially protein, can interfere with absorption by triggering digestive enzymes that break these supplements down too early.
Dosing Nattokinase and Lumbrokinase for Microclot Treatment
Nattokinase
Typical dose: 2,000 to 4,000 FU (fibrinolytic units) per day, divided into two doses
A single dose of 2,000 FU has been shown to increase fibrinolytic activity in humans (Kurosawa et al., 2005)
Best-studied form: NSK-SD®, a standardized nattokinase, free from vitamin K2, often used in research and safe for those on anticoagulant medications
Lumbrokinase
Maintenance dose: 1 capsule (typically 20 mg), 1–3 times per day
High-dose protocol: 2 capsules, 3 times per day (up to 6 capsules daily), often used short-term under medical supervision
Clinical research protocol: Some ongoing trials use 300,000 FU twice daily for 6 weeks in long COVID
Best-studied form: Boluoke® (Canada RNA), known for consistent potency, enteric coating, and widespread clinical use
Choose supplements from companies that list standardized enzyme activity and have undergone third-party testing or clinical use!
Safety, Side Effects, and When to Avoid Fibrinolytic Enzymes
Although nattokinase and lumbrokinase are natural compounds, they are pharmacologically active enzymes with strong effects on the body’s clot-dissolving system. For most people, they are well-tolerated. But in some cases, they may not be safe, especially for those with bleeding risks, multiple medications, or surgical plans.
When to Be Cautious with Nattokinase or Lumbrokinase
If you take blood thinners or antiplatelets
If you have active bleeding or recent surgery
In underweight or malnourished individuals
In children and teens
In pregnant women
Side Effects: What to Watch For
Most people tolerate nattokinase and lumbrokinase well, especially when taken correctly (on an empty stomach, with the right dose and formulation). Mild side effects may include:
Nausea or stomach upset (especially if taken with food)
Headache or dizziness (possibly due to vasodilation or clot resolution)
Minor bruising or prolonged bleeding from cuts (rare, but possible)
In research settings, both NSK-SD® (nattokinase) and Boluoke® (lumbrokinase) have shown no serious adverse events in healthy adults or cardiovascular patients when used at standard doses (Kim et al., 2008; Zhao et al., 2018).
Still, patients with ME/CFS or long COVID often have increased sensitivity to supplements. It’s best to start low and work with a knowledgeable clinician.
Vitamin K and Blood Thinner Interactions
Some nattokinase supplements contain vitamin K2, which can interfere with warfarin or affect blood INR levels. Choose products that are vitamin K-free, such as NSK-SD®, especially if you are on any blood-thinning medications.
Patients using prescription anticoagulants should monitor clotting markers regularly and consult their healthcare provider before starting any systemic enzyme.
Lumbrokinase and Nattokinase: Promising Tools for Microclot Treatment
Microclots are now recognized as a possible driver of symptoms in long COVID and ME/CFS, contributing to poor blood flow, low oxygen delivery, and persistent fatigue. While conventional treatments often miss this hidden clotting issue, enzymes like nattokinase and lumbrokinase offer a more targeted approach.
These fibrinolytic enzymes help break down fibrin—the main protein in microclots—and may improve circulation without the risks of standard anticoagulants. But for them to work, the formulation, timing, and dosing must be right. Clinical-grade products with proven bioavailability (like NSK-SD® and Boluoke®) are essential, and enzyme therapy should be used under medical guidance.
Although research in long COVID and ME/CFS is still in early stages, the mechanisms of these enzymes are compelling. Until large-scale trials are completed, nattokinase and lumbrokinase remain promising (but experimental) tools in managing microclot-related symptoms.
As part of an individualized, evidence-based strategy, they may offer real support for people living with complex postviral illness. Have you tried it? Tell us in the comments below.
References
Pretorius, E., Venter, C., Laubscher, G. J., Lourens, P. J., Steenkamp, J., & Kell, D. B. (2021). Persistent clotting protein pathology in Long COVID/Post-Acute Sequelae of COVID-19 (PASC) is accompanied by increased levels of antiplasmin. Cardiovascular Diabetology, 20(1), 172.
Pretorius, E., Maphumulo, S. C., Laubscher, G. J., & Kell, D. B. (2023). A proteomics-based analysis reveals anomalous clotting protein profiles in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). International Journal of Molecular Sciences, 24(1), 384.
Laubscher, G. J., Lourens, P. J., Venter, C., & Pretorius, E. (2021). COVID-19: Coagulopathy, thrombosis and the role of fibrinolysis. Seminars in Thrombosis and Hemostasis, 47(4), 406–414.
Wirth, K., & Scheibenbogen, C. (2020). A unifying hypothesis of the pathophysiology of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): Recognitions from the finding of autoantibodies against β2-adrenergic receptors. Frontiers in Neurology, 11, 373.
Grobbelaar, L. M., Venter, C., Vlok, M., Laubscher, G. J., Lourens, P. J., Steenkamp, J., & Pretorius, E. (2021). SARS-CoV-2 spike protein S1 induces fibrin(ogen) resistant to fibrinolysis: Implications for microclot formation in COVID-19. Bioscience Reports, 41(8), BSR20210611.
Sumi, H., Hamada, H., Nakanishi, K., & Hiratani, H. (1987). Enhancement of the fibrinolytic activity in plasma by oral administration of nattokinase. Acta Haematologica, 84(3), 139–143.
Dabbagh, F., Negahdaripour, M., Hoseinikhah, S., et al. (2022). Nattokinase: A promising alternative in prevention and treatment of cardiovascular diseases. Biomedicine & Pharmacotherapy, 148, 112749.
Hsu, R. L., Lee, K. T., Chen, Y. C., & Chen, C. S. (2009). The proteolytic activity of nattokinase and its effect on fibrinolysis. Biological Chemistry, 390(6), 495–500.
Kim, J. Y., Gum, S. N., Paik, J. K., et al. (2008). Effects of nattokinase on blood pressure: A randomized, controlled trial. Hypertension Research, 31(8), 1583–1588.
Kurosawa, Y., Nirengi, S., Homma, T., Esaki, K., Ohta, M., & Clark, J. F. (2005). A single-dose of oral nattokinase potentiates thrombolysis and anti-coagulation profiles. Scientific Reports, 5, 11601.
Zhang, G., Ma, X., Jiang, H., et al. (2013). Clinical observation of lumbrokinase in treating acute ischemic stroke. Chinese Journal of Integrative Medicine, 19(5), 346–351.
Yan, X., Jin, H., Zhang, R., et al. (2015). Identification of fibrinolytic proteins in the earthworm Lumbricus rubellus. PLoS ONE, 10(2), e0117223.